Repeat ECG Exams: A Thing of the Past?
Many major hospital systems across the U.S. are reporting losses in revenue due to short staffing, raised expenses, and poor investment performance.1 Some of the country’s largest for-profit hospital operators all reported a decrease in net income for the second quarter, compared with the same quarter the previous year.
In the diagnostic cardiology world, it is important to consider what optimizations can be made to turn this unfortunate trend around. What can save time? What can help lift the financial burden? The ECG exam is among the most routine diagnostic tests, but it is both time-consuming and resource intensive. Acquiring an ECG is a task commonly repeated due to many factors, which negatively impact patient and staff satisfaction and, worse yet, can delay critical intervention and treatment.
Save time with devices designed to capture accurate, diagnostic-quality data the 1st time around.
Learn more
Reasons Why Repeat ECGs Occur
According to a research study on file at Baxter2, physicians identified several common factors for requesting a repeat ECG acquisition. The presence of motion artifact, poor electrode quality, and improper patient prep/lead placement were among the top mentioned reasons.
- Poor staff training can result in improper prep/lead placement
- Using nonconforming or expired / dried up electrodes can impede the ECG signal
- Using worn out supplies such as adapter clips or lead wires can cause artifact
- Proximity to imaging equipment or mobile devices can impede the electrical signal on an ECG
Technology Helps Mitigate Repeat ECGs
It is important to ensure your acquisition devices are using technology to help you mitigate the above-referenced factors. Do you trust your ECG device’s algorithm? Do your devices have technology such as Best 10, which automatically selects the cleanest and best 10 seconds of ECG data from memory?
Avoid Repeat ECGs in the Acute Care Setting
Chest pain and shortness of breath are two of the leading ER diagnoses3 in the Emergency Department, and as the standard of care for determining, seemingly small delays in accurate ECG capture and delivery can delay critical patient care. Provider organizations across the care continuum are still plagued by rising expenses and labor shortages. To mitigate the effects of the labor shortage, most CFOs and revenue cycle VPs are turning to automation and technology.3
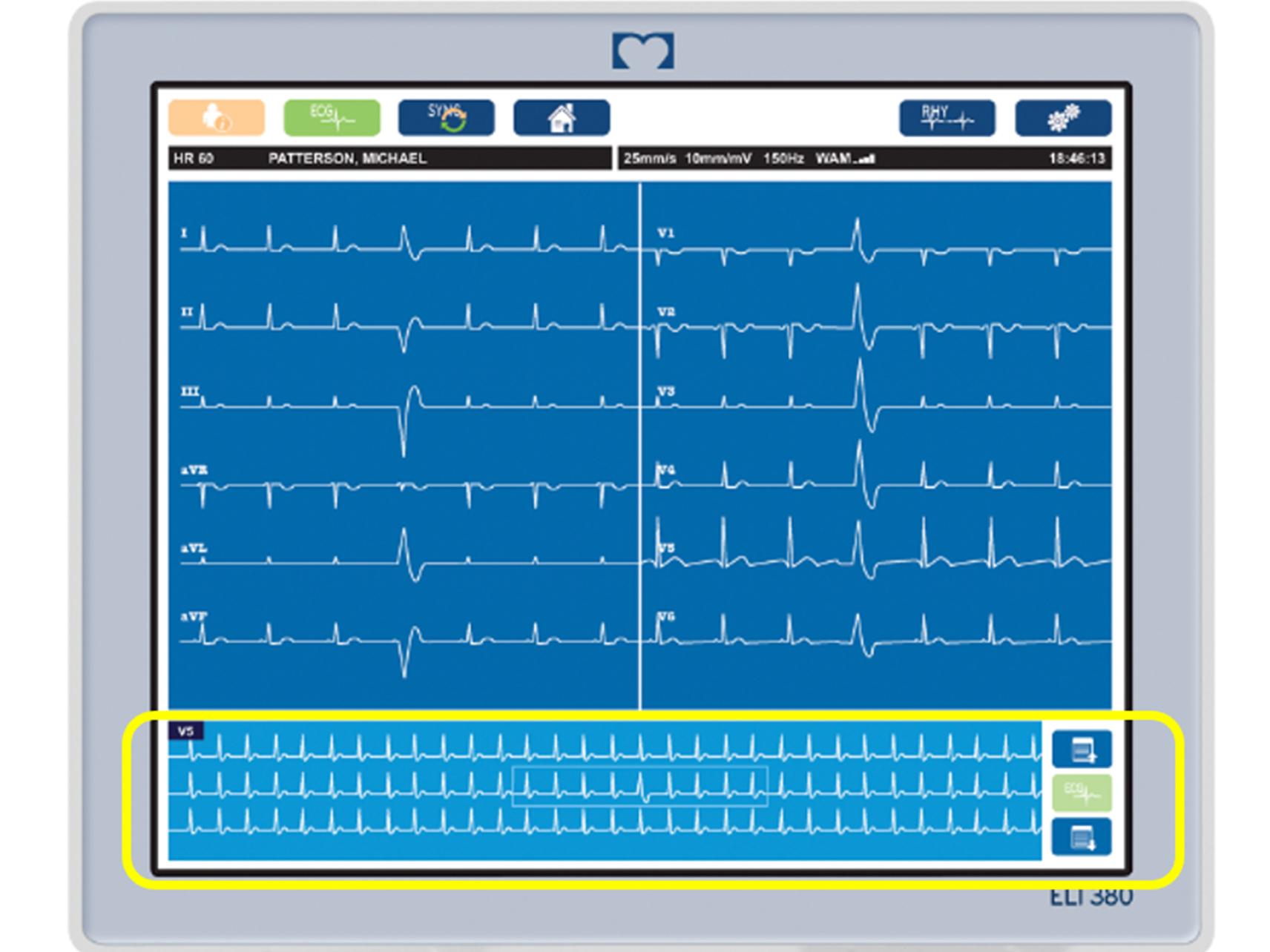
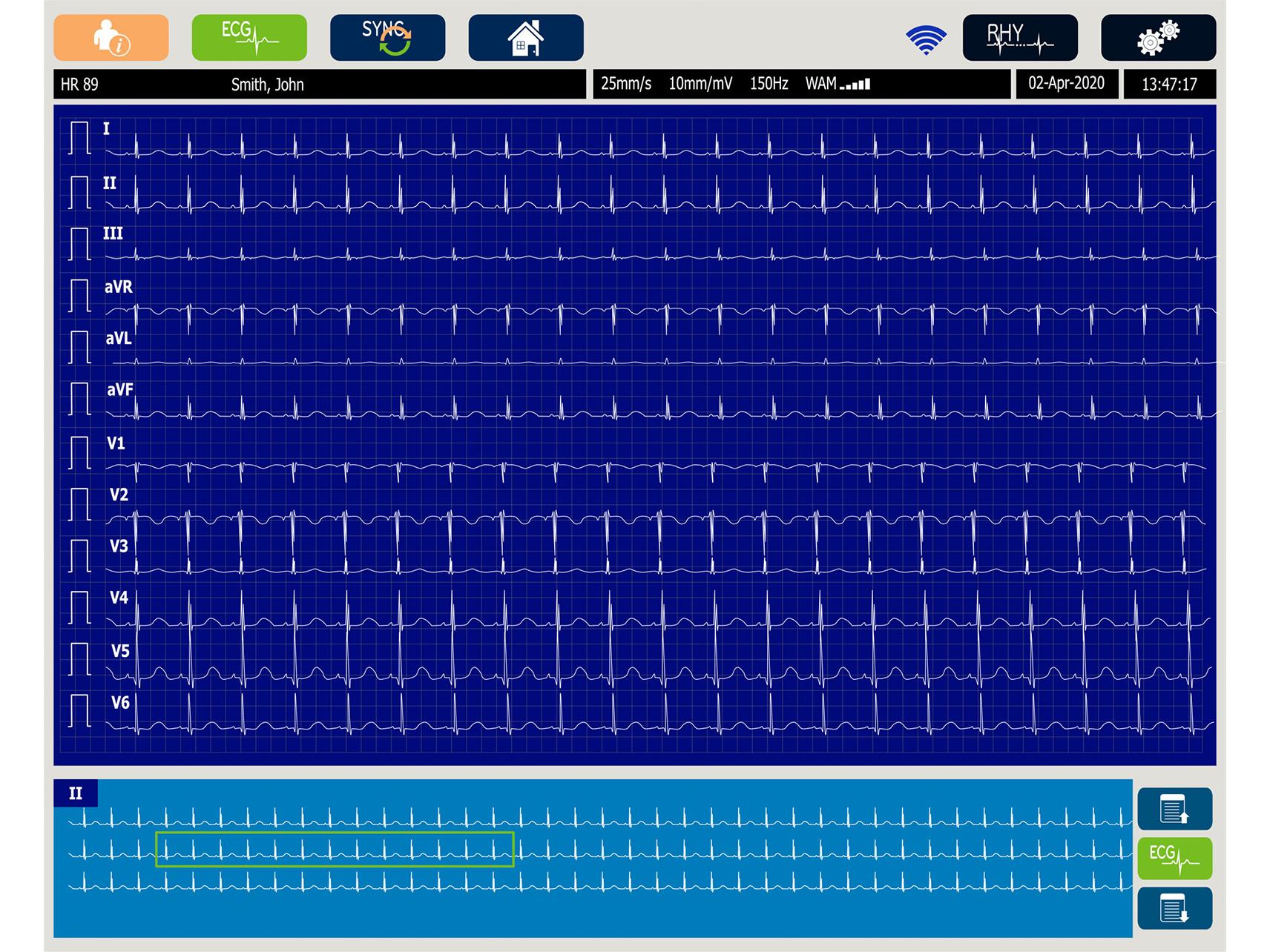
The ELI 380 Resting Electrocardiograph automatically captures the Best 10 seconds of ECG data from memory. Also, the device offers Full Disclosure, which provides continuous ECG data at the point of patient hookup automatically. When the caregiver captures the ECG, the technology will look back at the entire recording duration to select the cleanest, artifact-free rhythm that was recorded. This can help offset motion or environmental artifact that is so common, and ensure the caregiver captures a quality ECG signal that a physician can quickly read.
Best 10 seconds of ECG data
Full Disclosure: Continuous ECG for 20 minutes
To be as efficient as possible, your organization should have a process to ensure studies are immediately available in the EMR. With Baxter’s ELI 280 or ELI 380 resting ECG, securely transmit ECG data directly to your data management system or EMR with HL7, DICOM, or XML connectivity options.
Using less-than-stellar devices with a lack of connectivity could cause delayed results in the EMR and could incorrectly indicate that studies have not yet been performed when they already have.
SEE THE DEVICES IN ACTION
Schedule a Live, Customized Virtual Demo
Avoid Repeat ECGs in the Primary Care Setting
A repeat ECG research study on file at Baxter2 reported an 11% total repeat prevalence among primary care physicians, making this task much more common than in the acute care setting. Results reported that physicians were presented an ECG with artifact/poor-quality 19% of the time, causing a repeat exam 58% of the time.
26% of end users in primary care reported that they chose to repeat an ECG acquisition on their own prior to showing the primary care provider. If they were using devices they trusted to provide clean, accurate results the first time around, there would be no need for another exam. An average of 17%, physicians are provided with ECG results with artifact and/or poor quality.
Baxter’s Diagnostic Cardiology Suite intended for primary care is especially designed for improving diagnostic confidence as the device also utilizes the top-performing VERITAS algorithm and Best 10 functionality, automatically capturing the best 10 seconds of data. Reduce manual data entry and streamline your workflows. A clinician launches the Diagnostic Cardiology Suite from their EMR to perform an exam. An ECG is captured and saved for physician review, editing and signature, and then a final report with discrete data is uploaded to your EMR in the patient’s chart.
A Good Reason to Repeat ECGs, But Why They’re No Longer Necessary
Incorrect lead placement is very different in the eyes of the provider vs. the acquirer. According to an article from Pulsara6, incorrect lead placement is the main reason to obtain a repeat ECG. Baxter’s acute diagnostic and ambulatory cardiology devices offer a visual alert for lead swap right on the device, as well as a guide for correct lead placement.
Best Ways to Prevent Repeat ECG Exams
Perhaps it is time to consider investing in top-performing technology offering features to perform accurate ECGs the correct way the first time around, such as Baxter’s Best 10 feature, Full Disclosure, and VERITAS algorithm. The Best 10 feature is the top solution in both acute and primary care settings to prevent repeat ECGs.2 Investing in better technology can reduce manual data entry and automate diagnostic cardiology processes, often resulting in earlier diagnosis and treatment. Baxter’s devices are simple to use and have workflows for multiple user types, such as a technician, nurse, or physician.
The ECG is the most performed cardiovascular diagnostic procedure, with >100 million ECGs obtained annually in the United States.7 Reducing repeat ECG exams is one way to help prevent revenue loss and enable earlier diagnosis and treatment in the diagnostic cardiology department.